Explore RSV infection insights, ACOG’s vaccine guidelines, high-risk group impacts, care plan integration, and future prevention strategies in this comprehensive guide.As respiratory syncytial virus (RSV) continues to pose significant health risks, especially among vulnerable populations, the recent recommendations from the American College of Obstetricians and Gynecologists (ACOG) regarding RSV vaccination have sparked important conversations in the medical community. Understanding RSV infection and its implications is crucial for healthcare providers and expectant mothers alike. ACOG’s updated vaccine guidelines aim to enhance protection against RSV, particularly for high-risk groups, including infants and pregnant individuals. In this blog post, we will delve into ACOG’s vaccine recommendations, explore their impact on those at heightened risk, and discuss practical strategies for incorporating the RSV vaccine into care plans. Finally, we will consider future directions in prevention efforts to combat this respiratory virus effectively. Join us as we navigate the evolving landscape of RSV vaccination and its critical role in safeguarding health.
Understanding RSV Infection
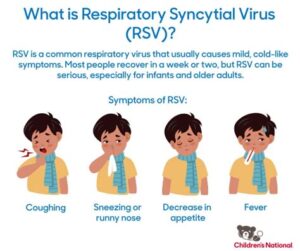
Respiratory Syncytial Virus (RSV) is a common respiratory virus that primarily affects infants and young children, but it can also impact adults, especially those with compromised immune systems or underlying health conditions. This virus is known to cause bronchiolitis and pneumonia, which can lead to severe respiratory complications, particularly in high-risk groups.
RSV spreads through respiratory droplets when an infected person coughs or sneezes. It can also survive on surfaces, making it easy to contract in environments such as daycare centers or crowded facilities. Symptoms typically manifest as a cold-like illness with cough, runny nose, and sometimes fever. In more severe cases, patients may experience wheezing and difficulty breathing.
Given the significant health implications of RSV, especially among high-risk populations, understanding the severity and transmission of the virus is crucial for developing effective prevention strategies. This is where guidelines from health organizations, such as the ACOG, regarding vaccination play an essent
ACOG’s Vaccine Guidelines
The American College of Obstetricians and Gynecologists (ACOG) has established comprehensive guidelines regarding the administration of the RSV (Respiratory Syncytial Virus) vaccine. These guidelines are particularly crucial for pregnant individuals and their infants, as RSV can lead to severe respiratory illnesses in young children.
ACOG recommends that healthcare providers educate their patients about the importance of the RSV vaccine and discuss its benefits. The guidelines stress administering the vaccine during specific times, especially during RSV season, which typically peaks in the fall and winter months.
Furthermore, the guidelines emphasize incorporating the RSV vaccine into care plans for high-risk groups, such as premature infants or those with underlying health conditions. This targeted approach aims to enhance the vaccine’s effectiveness and reduce the incidence of severe RSV-related illnesses in vulnerable populations.
Impact on High-Risk Groups
Respiratory Syncytial Virus (RSV) is a leading cause of respiratory illness in infants and young children, particularly in high-risk groups. The Centers for Disease Control and Prevention (CDC) identifies several populations that are particularly vulnerable to severe RSV infections, including preterm infants, children with chronic lung disease, and those with congenital heart defects. Understanding the impact of RSV on these groups is crucial for implementing effective prevention strategies.
The ACOG vaccine guidelines emphasize the urgent need for vaccination among vulnerable populations. Infants born prematurely, specifically those born at less than 29 weeks of gestation, are at a substantially higher risk. Research indicates that these infants experience not only more severe RSV infections but also face challenges during their recovery phases. Recommendations suggest that preventative measures, including vaccines, must be prioritized for these infants before their first RSV season.
Furthermore, children with underlying health conditions such as asthma or other pulmonary issues are also at heightened risk of severe RSV outcomes. It is essential for healthcare providers to assess the individual risk factors when designing care plans for these patients. By integrating RSV vaccines into regular health check-ups, we can mitigate risks associa
Incorporating RSV Vaccine into Care Plans
Incorporating the RSV vaccine into patient care plans is crucial for improving health outcomes in vulnerable populations, particularly infants and older adults. As the awareness of respiratory syncytial virus (RSV) continues to grow, healthcare providers are increasingly focused on the effective integration of preventive measures, including vaccination, into routine care. To ensure the RSV vaccine reaches those most in need, it is essential to develop comprehensive strategies that prioritize high-risk groups.
Healthcare professionals can start by assessing the risk factors associated with RSV among their patients. This assessment can be guided by established protocols that focus on age, underlying health conditions, and exposure risks. It is paramount to create a personalized care plan that includes vaccination as a key component for those who are identified as at risk. Family education becomes vital here; healthcare providers should explain the benefits of the RSV vaccine, potential side effects, and the importance of timely vaccination.
Furthermore, collaboration among healthcare teams is essential for the seamless incorporation of the RSV vaccine into care plans. This collaboration can be facilitated through systematic reminders for vaccination, tracking patient vaccination history, and ensuring open lines of communication regarding the importance of RSV immunization during regular check-ups. By prioritizing a proactive approach, we can enhance community awareness and ultimately minimize the impact of RSV infections.
Future Directions in Prevention Efforts
As we advance in the fight against RSV (Respiratory Syncytial Virus), innovative approaches to prevention efforts are essential. The landscape of healthcare is evolving, requiring us to adopt new methodologies to protect vulnerable populations from RSV infection. Research and clinical insights are guiding the development of effective strategies.
One promising direction is the integration of the RSV vaccine into universal immunization schedules. Studies have shown that early vaccination can significantly reduce the incidence of severe infections in high-risk groups, such as infants and the elderly. By prioritizing vaccination during routine healthcare visits, providers can enhance community immunity and lower the overall burden of RSV.
Additionally, further research into improving vaccine formulations and understanding viral mutations will play a critical role in addressing RSV. Collaborations between vaccine manufacturers, healthcare providers, and public health organizations can lead to expedited advancements in both preventive measures and treatment options, ensuring we are well-equipped to handle RSV in the future.
Frequently Asked Questions
What is the purpose of the ACOG RSV vaccine recommendation?
The ACOG RSV vaccine recommendation aims to provide guidance for the prevention of respiratory syncytial virus (RSV) infections, particularly targeting pregnant individuals to enhance immunity in infants.
Who does the ACOG recommend should receive the RSV vaccine?
The ACOG recommends that pregnant individuals receive the RSV vaccine during their third trimester to help protect their infants from RSV infections after birth.
When should the RSV vaccine be administered according to ACOG guidelines?
According to ACOG guidelines, the RSV vaccine should be administered during the third trimester of pregnancy, ideally between 32 and 36 weeks of gestation.
What are the benefits of the RSV vaccine for pregnant individuals?
The RSV vaccine for pregnant individuals offers the benefit of providing passive immunity to the newborn, reducing the risk of severe RSV infections in infants in their first months of life.
Are there any risks associated with receiving the RSV vaccine during pregnancy?
Currently, studies indicate that the RSV vaccine is generally safe for pregnant individuals; however, it is always important to consult with a healthcare provider to discuss specific health conditions and potential risks.
How effective is the RSV vaccine in preventing infections in infants?
The RSV vaccine has shown promise in clinical trials for significantly reducing the incidence of RSV infections and hospitalization rates among vaccinated infants.
What should healthcare providers consider when advising pregnant individuals about the RSV vaccine?
Healthcare providers should consider the current guidelines, individual health history, and any emerging evidence about the vaccine’s safety and effectiveness before advising pregnant individuals about the RSV vaccine.