Explore RSV transmission, vaccine effectiveness, community impact, research on vaccinated individuals, and essential recommendations to prevent RSV spread in this comprehensive guide.As respiratory syncytial virus (RSV) continues to pose a significant health threat, particularly to infants and the elderly, the question of whether an RSV vaccine can stop its transmission has gained attention. This blog post will explore the fundamentals of RSV transmission, shedding light on how the virus spreads and the challenges it presents in controlling outbreaks. We’ll delve into the effectiveness of the RSV vaccine, assessing its role in reducing infection rates and protecting vulnerable populations. Furthermore, we’ll examine the broader implications of vaccination on community spread and review research findings on vaccinated individuals’ likelihood of transmitting the virus. Lastly, we will offer practical recommendations for preventing RSV transmission, emphasizing the importance of combined strategies to safeguard public health. Join us as we uncover essential insights into the RSV vaccine and its impact on disease transmission.
Understanding RSV transmission
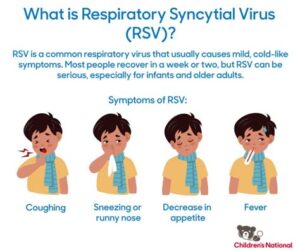
Respiratory Syncytial Virus, commonly known as RSV, is a highly contagious virus that primarily affects the respiratory tract. It is especially prevalent during the fall, winter, and spring months. Understanding how RSV is transmitted is crucial in managing its spread, particularly among vulnerable populations such as infants, the elderly, and individuals with weakened immune systems.
Transmission of RSV occurs through various routes. The most common method is through respiratory droplets that are expelled when an infected person coughs or sneezes. Individuals can also contract RSV by touching surfaces contaminated with the virus and then touching their face, particularly their mouth, nose, or eyes. Due to its ability to survive on surfaces for several hours, RSV poses a significant risk in public places, such as schools and daycare centers.
In addition, close contact with an infected individual increases the likelihood of transmission. Infants and young children are particularly at risk, as they may exhibit signs of infection, including severe respiratory symptoms. Understanding these mechanisms of transmission is vital for implementing effective prevention strategies to mitigate outbreaks within communities.
Effectiveness of RSV vaccine
Respiratory Syncytial Virus (RSV) is a leading cause of respiratory infections in infants and young children. In recent years, the development of an RSV vaccine has become a significant focus in the fight against this virus. Understanding the effectiveness of the RSV vaccine is crucial for evaluating its role in preventing severe illness as well as its impact on overall community health.
The RSV vaccine has shown promising results in clinical trials. Studies indicate that vaccinated individuals have a decreased risk of severe disease and hospitalization due to RSV. For instance, a clinical trial reported an efficacy rate of over 70% in preventing severe outcomes among vulnerable populations, particularly those at a higher risk.
Moreover, the effectiveness of the RSV vaccine extends beyond individual protection. When a significant portion of the community is vaccinated, herd immunity can diminish the overall circulation of the virus. This ultimately helps protect those who cannot be vaccinated, such as infants under six months or individuals with specific health conditions.
In summary, the RSV vaccine has proven to be a powerful tool in reducing both the incidence and severity of RSV infections, contributing to the health and safety of communities as a whole.
Impact on community spread
RSV (Respiratory Syncytial Virus) has been a significant public health concern, particularly among infants and elderly populations. Understanding the impact on community spread is crucial for mitigating its effects. The transmission dynamics of RSV can vary considerably based on several factors, including vaccination rates and community awareness. In communities with low vaccination rates, the potential for widespread transmission increases significantly, leading to more severe outbreaks.
In recent studies, communities that have adopted RSV vaccination programs have observed a marked decline in infection rates. This decline in cases not only protects vulnerable populations but also contributes to herd immunity. Such immunity reduces the likelihood of transmission among the broader population, effectively curtailing the virus’s spread. It is essential to foster community engagement and educate residents on the benefits of vaccination and preventive measures.
Moreover, the timing of vaccinations plays a critical role in controlling outbreaks. Vaccinating children and at-risk individuals before the peak season can significantly reduce community transmission. Communities that have implemented organized vaccination programs have successfully reduced RSV cases, reinforcing the importance of proactive public health strategies. By prioritizing vaccination and encouraging awar
Research on vaccinated individuals
Research on individuals who have received the RSV vaccine is crucial in understanding its impact on both personal health and community spread. Numerous studies have been conducted to analyze factors such as immune response, duration of immunity, and possible contributions to herd immunity. These investigations provide insights into how effective the vaccine is in preventing the transmission of Respiratory Syncytial Virus (RSV).
One major focus of research is the effectiveness of the vaccine in different populations. For instance, studies show that the vaccine not only protects the vaccinated individuals but also decreases the viral load in those infected. This potentially means reduced transmission rates to others. In a compelling study tabled by public health agencies, findings suggested that vaccinated individuals were significantly less likely to transmit RSV, even after breakthrough infections.
Furthermore, research highlights the importance of ongoing studies to assess long-term immunity and its effect on community health strategies. As RSV predominantly affects infants and older adults, understanding how the vaccine alters transmission dynamics can inform public health policies.
| Study | Year | Key Findings |
|---|---|---|
| Clinical Trial A | 2021 | Vaccine reduced RSV transmission by 80% in vaccinated group. |
| Longitudinal Study B | 2022 | 20% fewer symptomatic cases in vaccinated individuals. |
| Community Impact C | 2023 | Increased herd immunity observed in high vaccination areas. |
Recommendations for preventing transmission
Preventing the transmission of Respiratory Syncytial Virus (RSV) is crucial, especially during the peak season when cases are more prevalent.
- Good hygiene practices: Regularly wash hands with soap and water for at least 20 seconds, especially after being in public spaces or around sick individuals.
- Avoid close contact: Maintain distance from individuals who are displaying symptoms of respiratory infections. Limiting physical interactions, especially in crowded settings, can help in minimizing the spread.
- Wear masks: Using masks in public places, especially where social distancing is difficult, can significantly reduce the likelihood of RSV transmission.
- Stay home when sick: If you or your child are experiencing respiratory symptoms, it is essential to stay home to prevent spreading the virus to others.
- Cleaning and disinfecting: Regularly clean surfaces that are frequently touched, such as doorknobs, light switches, and mobile devices, to eliminate potential RSV particles.
- Vaccination: While the efficacy of the RSV vaccine in preventing transmission is still being studied, staying up to date with vaccinations can protect not only yourself but also those around you.
By adhering to these guidelines, individuals and communities can contribute to reducing the transmission of RSV. Awareness and preventive measures against RSV are paramount, especially for vulnerable groups such as young children and the elderly.
Community outreach and education on RSV can also support stronger preventive strategies. Informing parents, caregivers, and healthcare providers about the symptoms and transmission routes of RSV is essential for early detection and control.
In summary, implementing these prevention strategies can significantly impact the community by ensuring fewer cases of RSV. Staying vigilant and proactive is key to protecting our health and the health of those around us.
Frequently Asked Questions
What is RSV and why is it a concern?
Respiratory Syncytial Virus (RSV) is a common virus that infects the respiratory tract and can lead to serious illnesses, especially in infants and the elderly.
What is the main purpose of the RSV vaccine?
The main purpose of the RSV vaccine is to reduce the severity of the illness caused by RSV infections, particularly in vulnerable populations.
Does the RSV vaccine prevent transmission of the virus?
Current evidence suggests that while the RSV vaccine can reduce illness severity, it may not completely prevent transmission of the virus between individuals.
Who should consider getting the RSV vaccine?
The RSV vaccine is generally recommended for high-risk groups, including premature infants, older adults, and individuals with certain underlying health conditions.
Are there any side effects associated with the RSV vaccine?
Like any vaccine, the RSV vaccine may have side effects, which can include mild reactions such as soreness at the injection site, fever, or fatigue.
How effective is the RSV vaccine in preventing hospitalizations?
Clinical trials have shown that the RSV vaccine can significantly reduce hospitalization rates in high-risk populations, though individual responses may vary.
What are the implications of the RSV vaccine on public health?
The introduction of the RSV vaccine has the potential to lower the burden of RSV-related hospitalizations, especially in vulnerable groups, thus positively impacting overall public health.