Explore the RSV vaccine’s mechanism, effectiveness timeline, immune response, and expert recommendations for optimal timing to protect against respiratory infections.Respiratory Syncytial Virus (RSV) is a common but potentially serious infection, particularly for young children and the elderly. As awareness of RSV grows, so does the importance of understanding the RSV vaccine, which is designed to provide crucial protection against this virus. In this blog post, we’ll delve into how this vaccine works, its effectiveness timeline, and the immune response it generates. We will also offer guidance on when to get vaccinated, ensuring that you and your loved ones are well-informed about the best ways to safeguard against RSV. Join us as we explore the nuances of the RSV vaccine and its role in public health.
Understanding RSV vaccine
Respiratory Syncytial Virus (RSV) is a major cause of respiratory illness, particularly in infants and young children. The RSV vaccine aims to provide protection against this virus by stimulating the body’s immune response. This introduction of the vaccine is crucial as it helps to reduce hospitalizations and severe cases related to RSV infections.
Current developments in the field of RSV vaccines have shown promise. Two primary types of vaccines are being researched: live attenuated vaccines and inactivated (or killed) vaccines. Live attenuated vaccines involve using a weakened form of the virus, while inactivated vaccines contain killed virus particles. Both types work to expose the immune system to the virus, teaching it to recognize and combat future infections.
Clinical trials continue to assess the effectiveness and safety of these vaccines. Some studies indicate that the RSV vaccine may confer immunity within a few weeks after administration. However, achieving full effectiveness often requires a series of doses, making it essential to adhere to vaccination schedules recommended by healthcare providers.
Mechanism of vaccine action
The RSV (Respiratory Syncytial Virus) vaccine operates by harnessing the immune system’s natural ability to defend against infections. At its core, the vaccine introduces a harmless component of the virus, or a weakened version of it, to prompt an immune response without causing the disease itself.
Upon vaccination, the body identifies this component as a potential threat, initiating a series of biological processes. This involves the activation of B cells, which produce antibodies specifically designed to target RSV. Additionally, T cells play a crucial role in recognizing and destroying infected cells, ensuring a rapid and effective response during actual RSV exposure.
Once vaccinated, the immune system retains a “memory” of the RSV components. This immune memory allows the body to react swiftly and efficiently if it encounters the virus in the future, substantially reducing the severity of illness. Studies have shown that this mechanism can provide protection for several months, maki
Clinical effectiveness timeline
The RSV vaccine has been a significant development in the fight against respiratory syncytial virus (RSV), particularly for high-risk populations. Understanding the clinical effectiveness timeline is crucial for healthcare providers and patients alike. The vaccine’s effects are not instantaneous, and gauging when it begins to offer protection can guide vaccination strategies.
According to recent clinical studies, the vaccine demonstrates a marked reduction in RSV infections typically starting around two weeks post-administration. During this period, the body begins to build an immune response. The effectiveness of the vaccine tends to reach its peak roughly four to six weeks after vaccination, as indicated by a significant decrease in symptomatic cases among those vaccinated.
As the vaccine continues to work, its protection may last through the RSV season, which generally peaks in the winter months. Ongoing studies are essential to monitor the lasting effectiveness and any potential booster needs as the virus evolves. Understanding this timeline is essential for making informed decisions regarding immunization against RSV in vulnerable populations.
Immune response to vaccination
The immune response to the RSV vaccine is a key factor in its effectiveness and overall impact on public health. When the vaccine is administered, it stimulates the body’s immune system to recognize and combat the respiratory syncytial virus (RSV). The process begins with the introduction of weakened or inactivated virus components, which serve as antigens.
Upon vaccination, B cells and T cells are activated. B cells produce antibodies, which are proteins that specifically target the virus, preventing it from infecting cells. For those who may not be familiar with the terms, an antibody works like a lock and key: it locks onto the virus, neutralizing it and marking it for destruction. On the other hand, T cells play a crucial role in directly killing infected cells and orchestrating the broader immune response.
The duration and strength of the immune response can vary based on numerous factors, including age and overall health. Research indicates that the protective effects of the vaccine can last for months, with the potential need for booster doses to sustain immunity in specific populations. Monitoring the immune response is pivotal in assessing the vaccine’s effectiveness and guiding public health recommendations.
Recommendations for vaccine timing
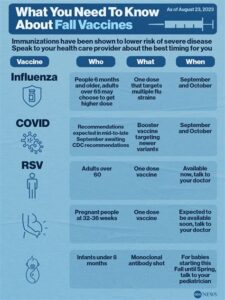
Understanding the timing of the RSV vaccine is crucial in maximizing its effectiveness. The timing recommendations can vary based on several factors, including age, health status, and seasonal outbreaks. Generally, it is advisable to administer the RSV vaccine during the late summer to early fall, prior to the onset of the RSV season, which typically peaks in the winter months.
For infants and young children, who are at a higher risk for severe RSV illness, healthcare providers often recommend getting vaccinated by the time they reach 6 months of age. This is particularly important for those with compromised immune systems or pre-existing respiratory conditions.
Additionally, for elderly individuals or those with chronic health issues, vaccination should occur in a timely manner, at the beginning of fall, to ensure they are well-protected before RSV strains begin to circulate widely in the community.
It is important to consult with healthcare professionals to determine the most suitable timing for vaccination based on individual risk factors and local epidemiological data. This strategy helps in achieving optimal immune response and preventing RSV infections effectively.
Frequently Asked Questions
What is the RSV vaccine?
The RSV vaccine is designed to protect against respiratory syncytial virus (RSV), a common virus that can cause serious respiratory illness, especially in infants and older adults.
How long does it take for the RSV vaccine to take effect?
The RSV vaccine typically starts to provide protection within a few weeks after administration, but full immunity may take longer.
Who is recommended to receive the RSV vaccine?
The RSV vaccine is generally recommended for infants, young children, and certain adults who are at high risk for severe RSV disease.
Are there any side effects associated with the RSV vaccine?
Like any vaccine, the RSV vaccine may cause side effects, which can include soreness at the injection site, mild fever, or fatigue, but serious side effects are rare.
Can adults receive the RSV vaccine?
Yes, certain adults, especially those over 65 or with underlying health conditions, may be recommended to receive the RSV vaccine to protect against severe illness.
How effective is the RSV vaccine?
Clinical trials have shown that the RSV vaccine can significantly reduce the risk of RSV-related hospitalizations and severe illness, particularly in high-risk groups.
How often should the RSV vaccine be administered?
The schedule for the RSV vaccine may vary based on the specific vaccine used and individual risk factors, so it’s important to consult a healthcare provider for personalized recommendations.