Explore the RSV vaccine, its types, effectiveness of live virus vaccines, and important considerations to ensure informed decisions about respiratory health.As the world grapples with the ongoing challenges posed by respiratory infections, the development of the RSV (respiratory syncytial virus) vaccine has garnered significant attention. Parents, healthcare professionals, and researchers are keen to understand not only the functionality but also the type of vaccine being introduced. This blog post delves into the nuances of the RSV vaccine, explores different vaccine classifications, and focuses particularly on the characteristics of live virus vaccines. We will dissect what a live virus vaccine entails, evaluate its effectiveness, and discuss key considerations surrounding the RSV vaccine. Join us as we unravel the science behind this vital development in respiratory health and shed light on its implications for our communities.
Understanding the RSV Vaccine
The Respiratory Syncytial Virus (RSV) vaccine is a critical tool in preventing severe respiratory infections caused by this virus, especially in vulnerable populations such as infants and the elderly. Understanding the RSV vaccine involves knowing its formulation, target populations, and the mechanism through which it provides protection against adenoviral infections.
Currently, there are a few candidates for the RSV vaccine that are in various stages of clinical trials. These vaccines primarily use two different approaches: live attenuated vaccines and subunit vaccines. Live attenuated vaccines contain a weakened form of the virus that can stimulate an immune response without causing disease, while subunit vaccines utilize specific parts of the virus to produce an immune response.
Live Virus Vaccines have been a topic of interest when discussing the RSV vaccine. Unlike traditional live virus vaccines that contain a weakened version of the pathogen they aim to protect against, the current RSV vaccine candidates may not be classified strictly as live virus vaccines. Ongoing research and trials will provide insights into their effectiveness and safety profiles.
In summary, understanding the potential benefits and limitations of the RSV vaccine is essential for ensuring public health, particularly in protecting high-risk groups.
Different Types of Vaccines
Understanding the different types of vaccines is crucial for grasping how they work in the immune system. Vaccines can be broadly classified into several categories, each with its unique mechanisms and advantages. In this section, we will explore the main types of vaccines, including live virus vaccines, inactivated vaccines, subunit vaccines, and mRNA vaccines.
1. Live Virus Vaccines: These vaccines use a weakened form of the virus that causes the disease. The weakened virus can replicate in the body and elicit a strong immune response without causing the disease. For example, the measles, mumps, and rubella (MMR) vaccine is a live virus vaccine that helps protect against these three diseases. However, because they contain live pathogens, there may be considerations for individuals with weakened immune systems.
2. Inactivated Vaccines: Unlike live virus vaccines, inactivated vaccines contain viruses that have been killed or inactivated, preventing them from causing disease. The inactivated poliovirus vaccine (IPV) is a notable example. These vaccines usually require multiple doses to achieve full immunity but are generally safer for people with compromised immune systems.
3. Subunit Vaccines: Subunit vaccines use only a part of the virus or bacteria, typically a protein, to stimulate an immune response. They do not contain live components and tend to have fewer side effects. The human papillomavirus (HPV) vaccine is an example of a subunit vaccine that provides effective protection against various cancer-causing strains.
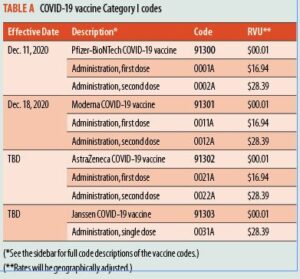
4. mRNA Vaccines: This newer type of vaccine uses messenger RNA to instruct cells to produce a harmless piece of the virus that triggers an immune response. The Pfizer-BioNTech and Moderna COVID-19 vaccines are prime examples. These vaccines do not use live virus and have been pivotal in combating the COVID-19 pandemic.
Understanding the different types of vaccines can aid in making informed decisions regarding immunization. Each type has its own set of benefits and considerations, particularly for at-risk populations. Whether considering the RSV vaccine or other vaccines, knowing how they function helps to appreciate their importance in maintaining health.
Live Virus Vaccines Explained
Live virus vaccines are an essential part of modern immunization strategies, particularly due to their effectiveness in training the immune system. Unlike inactivated vaccines, which use dead virus particles, live virus vaccines contain a weakened form of the virus that is still capable of replicating, but does not cause disease in healthy individuals.
- They often provide long-lasting immunity after just one or two doses.
- They stimulate a robust immune response, as the body recognizes the live virus and mounts a defense.
- They may cause mild symptoms similar to the disease, as the body reacts to the weakened virus.
Examples of live virus vaccines include the measles, mumps, and rubella (MMR) vaccine, as well as the yellow fever vaccine. These vaccines demonstrate how effectively live attenuated viruses can prepare the immune system to combat actual infections. Understanding these nuances helps in appreciating the broader scope of vaccination efforts aimed at preventing infectious diseases.
Effectiveness of Live Virus Vaccines
Live virus vaccines have been a cornerstone in the fight against various infectious diseases for decades. These vaccines contain a weakened form of the virus that causes disease, which enables the immune system to recognize and respond to the real virus should the body encounter it.
One of the main advantages of live virus vaccines is their ability to elicit a strong and lasting immune response. This is because the immune system is exposed to antigens in a way that mimics a natural infection, often resulting in the development of both humoral immunity (through antibody production) and cell-mediated immunity, which is critical for long-term protection.
However, the effectiveness of live virus vaccines can vary based on several factors, including the individual’s health status, age, and the specific virus involved. While they are often quite effective—providing immunity that may last for years or even a lifetime—there are still populations that may not achieve full immunity, such as those with compromised immune systems.
| Factors Influencing Effectiveness | Impact |
|---|---|
| Age | Infants and elderly may have reduced response |
| Health Status | Individuals with weakened immune systems may be less effective |
| Storage Conditions | Improper storage can reduce vaccine potency |
In summary, while live virus vaccines are a powerful tool in preventing infectious diseases, their effectiveness can be influenced by various factors. Policymakers and health professionals must consider these factors to optimize vaccination strategies and ensure broad community immunity.
Considerations for RSV Vaccine
When discussing the RSV vaccine, there are several key considerations that health professionals and the general public must take into account. Understanding these factors is crucial for making informed decisions about the vaccine’s usage, especially in vulnerable populations such as infants and the elderly.
One major consideration is the timing of vaccination. The RSV season generally peaks in the fall and winter months, and it is recommended that vaccination occur before the onset of this season to ensure maximum protection. Depending on the specific type of vaccine being developed or administered, different age groups may have varying recommendations.
Additionally, the safety and efficacy profile of the RSV vaccine must be thoroughly evaluated. Clinical trials play a pivotal role in identifying potential side effects and determining the vaccine’s overall effectiveness. Monitoring these outcomes in real-world settings will also provide invaluable data that can inform future vaccine strategies.
| Consideration | Description |
|---|---|
| Target Population | Infants, young children, and older adults are at higher risk for severe RSV infection. |
| Administration Schedule | Vaccination should ideally occur before RSV season starts. |
| Monitoring | Continual assessment of safety and efficacy during and after rollout. |
Ultimately, the considerations for the RSV vaccine encompass not only individual health outcomes but also broader public health implications. By addressing these considerations effectively, we can optimize the impact of the vaccine on RSV prevention and control.
Frequently Asked Questions
What is an RSV vaccine?
An RSV vaccine is designed to protect against respiratory syncytial virus (RSV), which is a common virus that causes respiratory infections in infants and young children.
Is the RSV vaccine a live virus vaccine?
No, the current RSV vaccines being developed are not live virus vaccines. They use inactivated virus or subunit technologies.
What are the benefits of the RSV vaccine?
The RSV vaccine aims to reduce the incidence of serious RSV infections, which can lead to hospitalizations and long-term respiratory issues in children.
Who should receive the RSV vaccine?
The RSV vaccine is primarily targeted at infants and young children, particularly those at high risk for severe RSV infections, such as premature babies or those with certain underlying health conditions.
When is the RSV vaccine expected to be available?
The RSV vaccine is currently in various stages of development, with some formulations expected to be available in the coming years as clinical trials are completed.
What are the side effects of the RSV vaccine?
Common side effects of the RSV vaccine may include mild fever, irritability, and pain at the injection site, but serious side effects are uncommon.
How does the RSV vaccine work?
The RSV vaccine works by stimulating the immune system to produce a protective response against the virus without causing the disease itself.