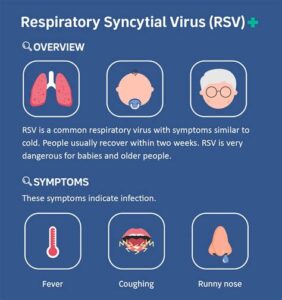
Discover the RSV vaccine: its function, effectiveness, side effects, and significant impact on public health. Learn how it protects vulnerable populations.As respiratory syncytial virus (RSV) continues to pose significant health risks, particularly to infants and the elderly, the development of an effective RSV vaccine is a groundbreaking advancement. This blog post delves into the essential aspects of the RSV vaccine, explaining what it is, how it operates, and its effectiveness in combating this viral threat. We will also explore potential side effects to be aware of and the broader implications of the vaccine on public health. With increasing awareness and vaccination efforts, understanding RSV and its vaccine is crucial for safeguarding vulnerable populations and promoting overall community health. Join us as we uncover the vital role this vaccine plays in protecting against a virus that affects millions worldwide.
What is the RSV vaccine?
The RSV vaccine is a medical intervention designed to provide protection against Respiratory Syncytial Virus (RSV), a common virus that can lead to severe respiratory infections, especially in infants and older adults. This vaccine is crucial because RSV is a leading cause of hospitalization in young children and can cause serious illness in vulnerable populations.
Currently, researchers are developing several formulations of the RSV vaccine, with different approaches aiming to elicit a strong immune response. The most promising candidates include live-attenuated vaccines, inactivated vaccines, and subunit vaccines, each with its own mechanism of action.
The vaccination strategy aims not only to protect individual patients but also to achieve herd immunity within communities, significantly reducing the overall incidence of RSV infections and associated healthcare burdens. As vaccination campaigns progress, understanding the implications of the RSV vaccine is more critical than ever.
How does the RSV vaccine work?
The RSV vaccine works by stimulating the body’s immune system to recognize and fight the respiratory syncytial virus (RSV), a common virus that can cause severe respiratory infections in infants and older adults. The vaccine contains inactivated or weakened components of the virus, which encourages the immune system to produce antibodies.
When a person receives the RSV vaccine, their immune system is trained to identify the virus more effectively in case of future exposure. This process is known as immunization, where the body learns to recognize the virus as a threat and mounts a defense against it. As a result, if the individual is later exposed to RSV, their immune system is prepared to act quickly to neutralize the virus, helping to prevent severe illness.
In clinical trials, researchers have monitored how well the RSV vaccine works in different populations, including infants and elderly individuals. The vaccine’s effectiveness may vary depending on several factors, including age, health status, and the specific strain of RSV. Nevertheless, this essential vaccination represents a significant advancement in the fight against RSV-related diseases.
Effectiveness of the RSV vaccine
The effectiveness of the RSV vaccine is an essential topic of discussion, especially when considering the impact on vulnerable populations, such as infants and the elderly. After extensive research and clinical trials, the vaccine has shown significant promise in reducing the incidence of respiratory syncytial virus (RSV) infections.
Studies have indicated that the RSV vaccine can reduce the risk of hospitalization among infants by up to 75%. This effectiveness is particularly noteworthy during RSV season, which typically peaks in the fall and winter months. The data gathered from Phase III trials reflects a strong immune response triggered by the vaccine, making it an effective tool in the fight against this virus.
Moreover, the RSV vaccine not only protects vaccinated individuals but also contributes to herd immunity. When a large portion of the population is vaccinated, the chances of spreading the virus are significantly lowered, thus protecting those who are unvaccinated or who cannot receive the vaccine due to medical contraindications. This community-wide protection is a vital aspect of public health efforts against infectious diseases.
Side effects of the RSV vaccine
The RSV vaccine has shown great promise in preventing respiratory syncytial virus infections, particularly in vulnerable populations such as infants and the elderly. However, like any vaccine, it is important to be aware of potential side effects that may arise following administration.
- Local reactions at the injection site, such as pain and swelling
- Fatigue
- Headaches
- Fever
- Mild rash
While these side effects are typically mild and resolve on their own within a few days, there may be rare, more serious adverse reactions. It is recommended that individuals consult with healthcare providers to weigh the benefits against the risks, especially when it comes to the vaccine for high-risk populations.
Impact of the RSV vaccine on public health
The introduction of the RSV vaccine marks a significant milestone in the battle against respiratory syncytial virus (RSV), particularly among vulnerable populations such as infants, the elderly, and individuals with weakened immune systems. The vaccine’s potential to reduce the incidence of severe RSV infections plays a crucial role in improving overall public health outcomes.
One of the most notable impacts of the RSV vaccine is its ability to decrease hospitalization rates associated with RSV infections. Studies have shown that widespread vaccination can lead to a substantial reduction in the number of children requiring hospitalization for serious respiratory illnesses. This not only alleviates the burden on healthcare facilities but also contributes to enhanced public health surveillance.
Furthermore, the vaccination against RSV has implications for herd immunity. As more individuals are vaccinated, the spread of the virus diminishes, which can protect those who are unvaccinated or those who cannot receive the vaccine due to health conditions. This collective immunity can lead to a significant drop in RSV cases, contributing to a healthier community overall.
Finally, beyond reducing healthcare costs related to RSV treatment, the vaccine generates a broader economic impact by allowing families to avoid lost wages due to illness and care responsibilities. In summary, the RSV vaccine is an essential tool in improving public health, reducing hospitalizations, and promoting community wellness.
Frequently Asked Questions
What is the RSV vaccine?
The RSV vaccine is designed to protect against respiratory syncytial virus (RSV), a common virus that can cause serious respiratory infections, particularly in infants and older adults.
Who should receive the RSV vaccine?
The RSV vaccine is primarily recommended for infants and young children at high risk of severe RSV infection, as well as older adults and individuals with weakened immune systems.
How does the RSV vaccine work?
The RSV vaccine works by stimulating the immune system to recognize and fight off the RSV virus, thereby preventing severe disease and complications associated with the infection.
What are the potential side effects of the RSV vaccine?
Common side effects of the RSV vaccine may include mild pain at the injection site, fever, irritability, or fatigue. Serious side effects are rare.
Is the RSV vaccine safe for pregnant women?
Current guidelines suggest that pregnant women should consult with their healthcare providers about the RSV vaccine, particularly if they are at high risk or have specific health concerns.
When is the best time to get vaccinated against RSV?
The best time to receive the RSV vaccine is typically before the start of the RSV season, which varies by region but usually occurs in the fall and winter months.
What is the effectiveness of the RSV vaccine?
The effectiveness of the RSV vaccine can vary based on age and health status, but clinical trials have shown promising results in reducing the incidence of severe RSV infections in high-risk populations.